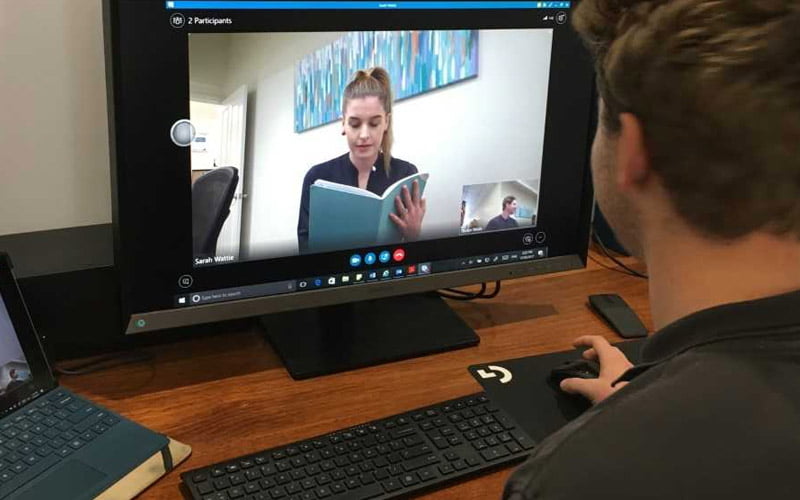
Telehealth refers to the use of technology to provide health services through phone conversations, emails and video conferencing such as Skype.
It allows us to provide a unique form of person-centered care that evidence suggests can be just as effective as a face-to-face session in the clinic. Below are some common myths about telehealth.
1. Telehealth is less effective than face-to-face sessions, and should only be used as a last resort.
There is strong agreement that telehealth has comparable outcomes to traditional face-to-face service delivery. Furthermore, research has found that telehealth has the advantage of delivering therapy in naturalized environments for the participant, which increases functional outcomes, addresses problems with generalising therapy to home environments and enhances participant satisfaction. This is because it takes therapy from being something that happens in the clinic and needs to be transferred over into the person’s life to something that is directly happening in the person’s life. Speech Pathology Australia has written a position paper on telehealth highlighting 75 articles that support the efficacy and effectiveness of telehealth across nearly all areas of speech pathology practice.
2. Telehealth is not as person-centered as face-to-face services.
In many ways telehealth allows for allied health practices to be more holistic than ever before. Research tells us that home and community-based therapy is the preference of people with disability and telehealth allows access to services for individuals who previously may have been restricted for reasons such as cost and distance. As mentioned above, providing therapy within the participant’s home has been shown to promote functional outcomes and increase satisfaction.
3. Participants do not like telehealth
There is a substantial body of research that demonstrates positive feedback and participant satisfaction with telehealth. From the beginning, the motivation for telehealth has been a desire to improve the delivery of rehabilitation services, and promote participant involvement in treatment.
Several factors have contributed to the development and implementation of telehealth.
These include:
- Rapid developments in technology. The increasing availability of smart devices are making telehealth more accessible to participants than ever before.
- Advances in neuroscience, which comes with new recommendations on the type, frequency and intensity of therapy.
- Increasing cost and demand for healthcare services.
- The need for equitable access to healthcare across metropolitan, rural, regional, and remote settings
Considering these factors, it’s easy to see why telehealth will continue to develop within health services.
There are many benefits of telehealth:
- Therapy can be delivered in natural environments. This allows for practice of goals within their desired context.
- Access to services regardless of location and transport options.
- Reduces travel time for the participant.
- Provides more opportunities to increase intensity of intervention.
- Allows the clinician to see how the participant is currently managing in their environment.
- Most people have access to a computer, tablet or smart device.
This form of health care delivery is not fool-proof and there are some limitations of telehealth. Not all participants have access to an internet connection while some assessments and therapies require a more ‘hands-on’ approach where direct interaction is most appropriate.
Telehealth is an exciting avenue for receiving services with a wealth of supporting research and participant satisfaction.